Category: Critical Care
Posted: 3/12/2024 by Quincy Tran, MD, PhD
(Updated: 5/3/2024)
Click here to contact Quincy Tran, MD, PhD
Background: There is no clear guidelines regarding whether norepinephrine or epinephrine would be the preferred agent to maintain hemodynamic stability after cardiac arrest. In recent years, there has been more opinions about the use of norepinephrine in this situation.
Settings: retrospective multi-site cohort study of adult patients who presented to emergency departments at Mayo Clinic hospitals in Minnesota, Florida, Arizona with out-of-hospital-cardiac arrest (OHCA). Study period was May 5th, 2018, to January 31st, 2022
Participants: 18 years of age and older
Outcome measurement: tachycardia, rate of re-arrest during hospitalization, in-hospital mortality.
Multivariate logistic regressions were performed.
Study Results:
Discussion:
It was retrospective study that uses electronic health records. Thus, other important factors from the pre-hospital settings might not be accurate.
On the other hand, the patient population came from multiple hospitals with varying practices so the patient population is more generalizable.
Conclusion:
Although the rate of tachyarrhythmia was not different between patients receiving norepinephrine vs. epinephrine after ROSC. This study would add more data to the current literature that norepinephrine might be more beneficial for patients with post-cardiac arrest shock.
Normand S, Matthews C, Brown CS, Mattson AE, Mara KC, Bellolio F, Wieruszewski ED. Risk of arrhythmia in post-resuscitative shock after out-of-hospital cardiac arrest with epinephrine versus norepinephrine. Am J Emerg Med. 2024 Mar;77:72-76. doi: 10.1016/j.ajem.2023.12.003. Epub 2023 Dec 10. PMID: 38104386.
Category: Ultrasound
Keywords: ultrasound, nerve block (PubMed Search)
Posted: 3/11/2024 by Alexis Salerno, MD
Click here to contact Alexis Salerno, MD
What happens if you have a patient who steps on a nail? How can you make this procedure easier for you and the patient?
– Use a Posterior Tibial Nerve Block! !
To Perform This Procedure:
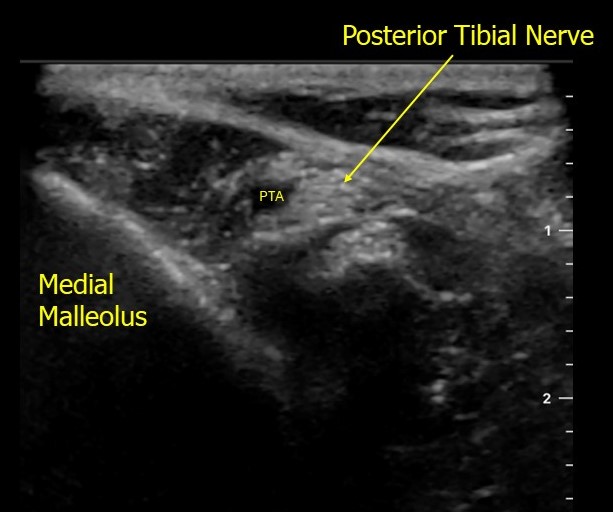
https://www.acep.org/patient-care/map/map-posterior-tibial-nerve-block-tool
Tibial — Highland EM Ultrasound Fueled pain management (highlandultrasound.com)
Category: Trauma
Posted: 3/10/2024 by Robert Flint, MD
(Updated: 5/3/2024)
Click here to contact Robert Flint, MD
This secondary analysis of the NEXUS head injury data found patients over 65:
-sustained more significant injuries than younger pts
-presented more frequently with occult injuries
-when they required neurosurgery intervention only 16% went home, 32% were discharged to rehab facility and 41% died
-mechanism of injury was most commonly fall from standing
-mortality rates were highest for fall from ladder and auto vs. pedestrian injuries
The authors concluded: “Older blunt head injury patients are at high risk of sustaining serious intracranial injuries even with low-risk mechanisms of injury, such as ground-level falls. Clinical evaluation is unreliable and frequently fails to identify patients with significant injuries. Outcomes, particularly after intervention, can be poor, with high rates of long-term disability and mortality.”
William R. Mower, Thomas E. Akie, Naseem Morizadeh, Malkeet Gupta, Gregory W. Hendey, Jake L. Wilson, Lorenzo Pierre Leonid Duvergne, Phillip Ma, Pravin Krishna, Robert M. Rodriguez,
Blunt Head Injury in the Elderly: Analysis of the NEXUS II Injury Cohort,
Annals of Emergency Medicine,
2024,
Category: Orthopedics
Posted: 3/8/2024 by Brian Corwell, MD
(Emailed: 3/9/2024)
(Updated: 5/3/2024)
Click here to contact Brian Corwell, MD
Acetaminophen and low back pain.
Acetaminophen has been a traditionally recommended first line intervention for acute low back pain.
Cochrane reviews in 2016 and 2023 found that acetaminophen showed no benefit compared to placebo in patients with acute low back pain.
A 2020 study investigated whether the addition of acetaminophen to short term NSAID therapy was beneficial.
A randomized double-blind study conducted in two urban emergency departments.
Patients randomized to a 1-week course of ibuprofen plus acetaminophen versus ibuprofen plus placebo.
Population: patients presenting with acute, non-radicular, non-traumatic lower back pain of fewer than two weeks duration.
Authors compared pain and functional outcomes at one week following discharge.
Conclusion: there was no outcome benefit from the addition of acetaminophen to ibuprofen.
Friedman BW, et al. Ibuprofen Plus Acetaminophen Versus Ibuprofen Alone for Acute Low Back Pain: An Emergency Department-based Randomized Study. Acad Emerg Med. 2020 Mar;27(3):229-235.
Category: Trauma
Posted: 3/3/2024 by Robert Flint, MD
(Updated: 5/3/2024)
Click here to contact Robert Flint, MD
This is a retrospective study looking at traumatic brain injury patients comparing those with and without pre-existing psychiatric illness at the time of injury. Those with pre-existing illness had longer hospital stays, longer ICU stays and more frequent readmissions.
Benavides F, Liporaci J, Getchell J, et al. Effects of pre-existing psychiatric illness on traumatic brain injury outcomes: A propensity-matched cohort study. Trauma. 2024;0(0). doi:10.1177/14604086231187157
Category: Quality Assurance/Quality Improvement
Keywords: Metacognition, Diagnostic Error (PubMed Search)
Posted: 3/2/2024 by Brent King
(Updated: 5/3/2024)
Click here to contact Brent King
This classic article should be on everyone’s reading list.
The Bottom Line: Clinicians engaging in metacognition, that is thinking about our reasoning process, can avoid making some critical errors and falling victim to cognitive biases.
Diagnostic errors are common in clinical medicine and particularly common in situations in which the clinician is faced with a novel circumstance and cannot, therefore easily apply heuristics or rules. There are also certain classic situations in which cognitive errors often occur (e.g., mistaking intracranial injury for intoxication). Through a process of active consideration of one’s diagnostic approach, many errors and cognitive biases (particularly availability bias and anchoring bias) can be avoided.
Take-home message: This article is worth reading in its entirety. Applying these principles can protect both patients and clinicians from the consequences of diagnostic errors.
Croskerry, P. Cognitive forcing strategies in clinical decision-making. Ann Emerg Med 2003;41:110-120
Category: Pediatrics
Posted: 2/29/2024 by To-Lam Nguyen, MD
(Emailed: 3/1/2024)
(Updated: 3/1/2024)
Click here to contact To-Lam Nguyen, MD
You've heard of one kill pills such as calcium channel blockers, beta blockers, sulfonylureas, anti-malarials, but less commonly known is benzonatate, or tessalon perles.
Tessalon perles are not recommended for children under the age of 10. 1-2 capsules of benzonatate in children <2 years old have been reported to cause serious side effects including restlessness, tremors, convulsions, coma and even cardiac arrest rapidly after ingestion (within 15-20 minutes and death within a couple of hours). It is attractive to young children as it somewhat resembles a jelly bean.
Pearls on Tessalon Perles:
https://www.poison.org/articles/are-benzonatate-capsules-poisonous
Thimann DA, Huang CJ, Goto CS, Feng SY. Benzonatate toxicity in a teenager resulting in coma, seizures, and severe metabolic acidosis. J Pediatr Pharmacol Ther. 2012 Jul;17(3):270-3. doi: 10.5863/1551-6776-17.3.270. PMID: 23258970; PMCID: PMC3526931.
Category: Trauma
Posted: 2/29/2024 by Robert Flint, MD
(Updated: 5/3/2024)
Click here to contact Robert Flint, MD
This meta analysis did not find convincing evidence for or against seizure prophylaxis for admitted moderate to severe traumatic brain injury pts. They recommend Levetiracetam over other medications again on weak evidence.
Frontera, J.A., Gilmore, E.J., Johnson, E.L. et al. Guidelines for Seizure Prophylaxis in Adults Hospitalized with Moderate–Severe Traumatic Brain Injury: A Clinical Practice Guideline for Health Care Professionals from the Neurocritical Care Society. Neurocrit Care(2024). https://doi.org/10.1007/s12028-023-01907-x
Category: Administration
Keywords: employee, independent contractor, employment, job market (PubMed Search)
Posted: 1/12/2024 by Steve Schenkel, MPP, MD
(Emailed: 2/28/2024)
(Updated: 2/28/2024)
Click here to contact Steve Schenkel, MPP, MD
The relationship between an Emergency Physician and the hiring group (whether large or small) may be one of employer-employee or contactor-independent contractor. There are legal job protections for employees that don’t exist for independent contractors. There are also regulations that define an independent contractor. Enforcement of these regulations varies but may be increasing. This has implications for the Emergency Medicine job market. We have the highest percentage of independent contractors of any medical specialty.
See more at Leon Adelman’s Emergency Medicine Workforce Newsletter, here https://emworkforce.substack.com/p/thousands-of-employed-emergency-physicians
Category: Hematology/Oncology
Keywords: Cancer, ACS, AMI, troponin (PubMed Search)
Posted: 2/26/2024 by Sarah Dubbs, MD
(Updated: 5/3/2024)
Click here to contact Sarah Dubbs, MD
Evidence is mounting that individuals with active or past history of cancer are at increased risk for acute cardiovascular events such as as acute myocardial infarction. This secondary analysis from the APACE (Advantageous Predictors of Acute Coronary Syndromes Evaluation) study- a multicenter, international, prospective diagnostic study looked at the prevalence of MI in patients with history of cancer presenting to the ED with acute chest pain, diagnostic accuracy of high-sensitivity troponins and diagnostic algorithms (European Society of Cardiology algorithm- see paper for details), among a few other parameters.
Take home points:
Translation to practice:
Be more conservative with cancer patients presenting to the ED with acute chest pain!
Bima, P, Lopez-Ayala, P, Koechlin, L. et al. Chest Pain in Cancer Patients: Prevalence of Myocardial Infarction and Performance of High-Sensitivity Cardiac Troponins. J Am Coll Cardiol CardioOnc. 2023 Oct, 5 (5) 591–609.
https://doi.org/10.1016/j.jaccao.2023.08.001
Category: Trauma
Keywords: Hip fracture l, hemoglobin l, mortality (PubMed Search)
Posted: 2/25/2024 by Robert Flint, MD
(Updated: 5/3/2024)
Click here to contact Robert Flint, MD
In this study, geriatric hip fracture patients with a hemoglobin less than 7.1 had higher mortality, especially in those over age 79, even when controlling for other factors such as ASA Physical status class, anti-platelet use, etc.
Bruce K, Mangram A, Sucher JF_, et al_
Consequences of anemia in geriatric hip fractures: how low is too low?
Trauma Surgery & Acute Care Open 2024;**9:**e001175. doi:10.1136/tsaco-2023-001175
Category: Orthopedics
Keywords: neck pain, radiculopathy (PubMed Search)
Posted: 2/24/2024 by Brian Corwell, MD
Click here to contact Brian Corwell, MD
Axial neck pain is a dull aching “soreness” pain from the posterior neck muscles with radiation to the occiput, periscapular and shoulder regions.
Associated with headaches, stiffness and muscle spasm.
Patients with cervical radiculopathy, however, usually present with unilateral pain discomfort.
Patients may complain of pain radiation into the ipsilateral arm. Though frequently difficult to describe, this may be in a dermatomal distribution. Patients may also report decreased sensation in a dermatomal distribution or weakness along the corresponding myotome.
The most affected nerve roots are C7 (C6-7 herniation), followed by C6 (C5-6 herniation) and C8 (C7-T1 herniation).
Cervical Spondylosis (degenerative change) is the most common ideology.
As discs breakdown with age and lose height, increased force loads are transmitted to bony regions of the spinal segment leading to bone hypertrophy which creates foraminal stenosis and resultant radiculopathy.
Cervical radiculopathy, like lumbar radiculopathy, is largely a self-limited condition. Several older studies following this diagnosis revealed that a majority of patients were either asymptomatic or mildly symptomatic at time of follow-up.
Improvement is seen over the initial four to six months following diagnosis.
Category: Administration
Posted: 2/22/2024 by Robert Flint, MD
(Updated: 5/3/2024)
Click here to contact Robert Flint, MD
This research letter notes: “The Rural Emergency Hospital is a new Medicare payment model available to hospitals with 50 or fewer beds in rural areas. Rural hospitals converting to this model will have emergency department (ED), observation, and outpatient services.”. Their study concludes that the majority of these hospitals already transfer the vast majority of their admissions to larger hospitals and this designation is a recognition of already established practices.
https://doi.org/10.1016/j.annemergmed.2023.08.492
RESEARCH LETTER| VOLUME 83, ISSUE 2, P177-180, FEBRUARY 2024
Category: EMS
Keywords: vital signs, age, pediatric, prehospital intervention (PubMed Search)
Posted: 2/21/2024 by Jenny Guyther, MD
(Updated: 5/3/2024)
Click here to contact Jenny Guyther, MD
Vital signs in children can be difficult to remember since they vary with age. Using a standardized card or app (such as PALS) can help EMS clinicians remember the values. Most pediatric vital sign reference ranges were derived from samples of healthy children in the outpatient setting (ie PALS). This study attempted to validate a range of pediatric vital signs that were more accurate in predicting the need for prehospital interventions compared to the standard PALS vital sign ranges. The thought was that by using EMS data, these vital sign ranges could better alert EMS to patients in need of acute intervention.
The authors used a large EMS database to determine the vital signs for the patients age and correlated that to prehospital interventions (including IV, medication, EKG, advanced airway management, ect). They used the <10% and >90% for the age values (termed "extreme" vitals signs) as a cut off to be considered abnormal. Using the EMS derived values, 17.8% of the encounters with an extreme vital sign received medication. If the PALS abnormal vital sign range was used, only 15.2% of those patients were given medications. Overall, encounters with an extreme vital sign had a higher proportion of any intervention being performed compared to other vital sign criteria (i.e. only 33.7% with PALS).
These extreme vital signs also had a greater accuracy in predicting mortality.
Bottom line: While vital signs are based on physiology that does not change based on location, using a seperate criteria for the EMS population, can improve discrimination between sick and sicker patients and hopefully allow EMS to recognize and intervene on sicker patients sooner.
Ramgopal S, Sepanski RJ, Crowe RP, Martin-Gill C. External validation of empirically derived vital signs in children and comparison to other vital signs classification criteria [published online ahead of print, 2023 Apr 27]. Prehosp Emerg Care. 2023;1-15. doi:10.1080/10903127.2023.2206473
Category: Critical Care
Keywords: poisoning, intoxication, altered mental status, GCS, endotracheal intubation (PubMed Search)
Posted: 2/20/2024 by Kami Windsor, MD
Click here to contact Kami Windsor, MD
Background: Acutely intoxicated / poisoned patients are commonly encountered in the ED, with the classic teaching that a GCS < 9 is an indication to intubate for airway protection. But we’ve probably all had a patient who was borderline, or who we thought was still protecting their airway pretty well despite a lower GCS. Are we risking our patient’s health and our careers by holding off on intubation? Maybe not.
The NICO trial, a multicenter, randomized controlled trial, looked at patients presenting by EMS with GCS <9 due to suspected poisoning, without immediate indication for intubation (defined by signs of respiratory distress with hypoxia, clinical suspicion of any brain injury, seizure, or shock with systolic BP <90 mmHg). They found that withholding intubation with close monitoring, compared to the standard practice of intubating at the EMS or ED physician’s discretion, resulted in:
Comparing the patients who were intubated in each group, there was no significant difference between groups in:
Notes:
Bottom Line: Without clear indication for intubation such as respiratory distress or accompanying head bleed, etcetera, intubation for mental status alone shouldn't be dogma in acute intoxication. Close monitoring will identify need for intubation, without apparent worsened outcomes due to a watchful waiting approach.
Freund Y, Viglino D, Cachanado M, et al. Effect of Noninvasive Airway Management of Comatose Patients With Acute Poisoning: A Randomized Clinical Trial. JAMA. 2023; 330(23):2267-2274. doi: 10.1001/jama.2023.24391.
Category: Trauma
Keywords: Pelvic binder, trauma, survival, mortality (PubMed Search)
Posted: 2/18/2024 by Robert Flint, MD
(Updated: 5/3/2024)
Click here to contact Robert Flint, MD
This retrospective study of 66 trauma patients who had pelvic fractures attempted to determine if prehospital applied pelvic binders had an impact on mortality. There were 3 cohorts: appropriately applied binders (14), inappropriately applied (14 not at the level of the greater trochanter), and none applied (38). Survival for applied was 92% and those without was 81% which was not statistically significant. The authors concluded: “In conclusion, our study found that the use of prehospital pelvic binders did not show a significant effect on patient outcomes for those with unstable pelvic fractures. Instead, injury severity score (ISS) emerged as the most significant predictor of survival.”
Previous studies have shown regular education is needed on proper use of binders. We should continue to educate on appropriate positioning and the use of pelvic binders. For me, this study is not large enough to convince that we should go away from binder use. We need more data before we abandon the pelvic binder.
Alonja Reiter, André Strahl, Sarina Kothe, Markus Pleizier, Karl-Heinz Frosch, Konrad Mader, Annika Hättich, Jakob Nüchtern, Christopher Cramer,
Does a prehospital applied pelvic binder improve patient survival?,
Injury,
2024,
111392,
ISSN 0020-1383,
Category: Pediatrics
Keywords: myositis, acute kidney injury, problems walking, calf pain (PubMed Search)
Posted: 2/14/2024 by Jenny Guyther, MD
(Emailed: 2/16/2024)
(Updated: 2/16/2024)
Click here to contact Jenny Guyther, MD
BACM stands for benign acute childhood myositis which is typically a benign, viral induced self limiting illness. This was a retrospective study looking at 65 patients in Italy to further characterize the characteristics of the disease.
In this study, the median patient age was 6 years with a male predominance. The incidence of BACM peaked in winter with a second peak in the fall. Patients presented with prodromal symptoms including fever, cough, coryza, sore throat and vomiting. The exam showed difficulty walking and myalgias with reproducible calf tenderness and preserved reflexes. Influenza B and A, COVID and other viral pathogens have been detected in these patients.
Lab work may show an elevated creatinine kinase, AST and potassium. WBC and CRP may also be elevated. The median CK value was 943 U/L and on average normalized within one week. Other studies have shown median CK values in the 3300s. Treatment includes hydration to promote CK clearance and prevent complications including acute kidney injury related to rhabdomyolysis. Recurrent myositis or CK values > 5000 U/L should have screening tests for muscular dystrophy and metabolic disorders.
Attainaese et al. Benign acute children myositis: 5 year experience in a tertiary pediatric hospital. European Journal of Pediatrics, published online July 18 2023.
Category: Toxicology
Keywords: bupropion, QRS widening, NaHCO3 (PubMed Search)
Posted: 2/15/2024 by Hong Kim, MD
(Updated: 5/3/2024)
Click here to contact Hong Kim, MD
Bupropion associated cardiac toxicity widens the QRS complex by inhibiting the cardiac gap junction, not cardiac Na channel blockade. NaHCO3 is often administered when EKG changes are noted. But the effectiveness of NaHCO3 in bupropion toxicity is not well established.
A retrospective study between 2010-2020 showed, that administration of NaHCO3 only decreased QRS duration by 2 msec (median). The median NaHCO3 administered was 100 mEq. Although this study was limited by the fact that it only had a small sample size of 13, NaHCO3 administration may provide limited clinical benefit in patients with QRS widening from bupropion overdose.
Simpson M et al. Sodium bicarbonate treatment for QRS widening in bupropion overdoses
Category: Gastrointestional
Keywords: ED recidivism, abdominal pain, follow up appointments (PubMed Search)
Posted: 2/14/2024 by Neeraja Murali
(Updated: 5/3/2024)
Click here to contact Neeraja Murali
How many times have you discharged a patient with a clinical impression of “abdominal pain” with no clear explanation or diagnosis?
How many of these times do you direct them to follow up with gastroenterology? And more importantly, how often do they actually do so?
This study discussed a multi-disciplinary approach to ensuring adequate follow up for patients, utilizing an EMR based transition of care (TOC) program. The study stratified patients into 2 groups, pre and post TOC program implementation, to assess rates of appointment scheduling and attendance, as well as rates of return to ED within 30 days. Patients were further stratified based on their Distressed Communities Index (DCI) score (a composite of 7 different socioeconomic metrics) into 5 tiers: Distressed Communities, At Risk Communities, Mid-Tier Communities, Comfortable Communities, and Prosperous Communities. Prior to the implementation of the TOC program, the onus was on the patient to schedule their appointment. The TOC program consisted of an order placed in EMR, which triggered review of the patient's chart by the gastroenterology attending or NP. This individual would then message the information to the appropriate GI subspecialty clinic, along with a time frame in which the patient should be seen. The clinic would then check the patient's insurance reach out to the patient directly to schedule the appointment.
While there was no signifcant difference in 30-day readmission between the pre and post TOC program patients, the post-implementation group was found to both schedule appointments (50% vs 27% p-value <0.01) AND show up to appointments (34% vs 24% p-value <0.01) at significantly higher rates compared to Pre-TOC patients. Additionally, post-TOC patients in the At-Risk and Distressed DCI groups were 22x more likely to follow up than the same groups in the pre-TOC group (OR 22.18, 95% CI 4.23–116.32).
Though the study had promising results, it did admittedly have some limitations, namely the size of the at-risk and distressed groups. Another consideration, though not mentioned in the paper, is that access to a working phone is necessary to the success of this program. Nevertheless, the idea of a TOC program is worth consideration as a means to ensure that patients are not lost to follow up and potentially reduce the risk of adverse events.
Mizrahi J, Marhaba J, Buniak W, Sun E. Transition-of-care program from emergency department to gastroenterology clinics improves follow-up. Am J Emerg Med. 2023;69:154-159. doi:10.1016/j.ajem.2023.04.030
Category: Administration
Keywords: Transfer, surgery, scoping review, further research (PubMed Search)
Posted: 1/28/2024 by Robert Flint, MD
(Emailed: 2/11/2024)
(Updated: 2/11/2024)
Click here to contact Robert Flint, MD
These authors performed a scoping review of English language studies involving United States general surgery patients that required transfer to another facility looking at timing of transfer, triage guidelines, and mode of transport . They concluded: “There were mixed results for the impact of transfer timing on outcomes with heterogeneous definitions of delay and populations. Triage guidelines for EGS transfer were consensus or expert opinion. No studies were identified addressing the mode of interfacility EGS transfer.” More research is needed in the area concerning timing, triage and mode of transport for these patients.
Silver, David S. MD, MPH; Teng, Cindy MD; Brown, Joshua B. MD, MSc. Timing, triage, and mode of emergency general surgery interfacility transfers in the United States: A scoping review. Journal of Trauma and Acute Care Surgery 95(6):p 969-974, December 2023. | DOI: 10.1097/TA.0000000000004011
