Category: Administration
Keywords: trauma, EMS, hemorrhagic shock (PubMed Search)
Posted: 5/3/2024 by Ben Lawner, MS, DO
Click here to contact Ben Lawner, MS, DO
BACKGROUND:
Prehospital administration of whole blood involves some areas of controversy. Though theoretical benefits are clear, concerns about logistics and timing of blood often dominates the discussion. This study was a retrospective analysis of prehospital blood administration within an urban EMS system from 2021-2023. Primary endpoints included: time to administration and in hospital mortality.
PATIENTS/METHODS:
The study population included patients presenting to the EMS system with signs and symptoms of hemorrhagic shock (SBP<70 or SBP<90 + HR> 100, n=61) and who received at least 1 unit of prehospital blood (PHB). The EMS system administered blood in conjunction with an advanced resuscitative bundle (calcium, TXA, blood). Isolated head injuries and blunt trauma patients were excluded from the analysis. The control group (n=82) was comprised of patients in the system's trauma registry presenting to EMS PRIOR to the initiation of whole blood and who exhibited similar clinical crtieria.
RESULTS:
BOTTOM LINE:
In this prospective study conducted within an urban EMS system, patients receiving prehospital whole blood demonstrated improved vital signs and reduced mortality when compared to a control group. Slightly extended prehospital time intervals for patients receiving PHB may be offset by the measured benefits of whole blood therapy.
Duchesne, J. , McLafferty, B. , Broome, J. , Caputo, S. , Ritondale, J. , Tatum, D. , Taghavi, S. , Jackson-Weaver, O. , Tran, S. , McGrew, P. , Harrell, K. , Smith, A. , Nichols, E. , Dransfield, T. , Marino, M. & Piehl, M. (9900). Every minute matters: Improving outcomes for penetrating trauma through prehospital advanced resuscitative care. Journal of Trauma and Acute Care Surgery, Publish Ahead of Print , doi: 10.1097/TA.0000000000004363.
Category: Obstetrics & Gynecology
Keywords: postpartum depression (PubMed Search)
Posted: 5/2/2024 by Michele Callahan, MD
(Updated: 5/3/2024)
Click here to contact Michele Callahan, MD
Perinatal mental health problems are unfortunately quite common: according to the World Health Organization, approximately 10% of women in high-income countries and approximately 30% in low- or middle-income countries are affected.
It's important to be able to distinguish “baby blues” from more significant mental health issues. Typical symptoms of the “baby blues” include mild and short-lived changes in mood, as well as feelings of exhaustion, worry, and unhappiness in the weeks that follow giving birth.
Symptoms that are more severe or lasting >2 weeks post-partum should prompt further investigation and discussion with a mental health professional. Symptoms of perinatal depression may include: feeling persistently sad, feelings of hopelessness, loss of interest or pleasure in hobbies/activities, trouble bonding with the infant, appetite changes, and can even become as severe as wanting to harm onself or one's child. There are specific DSM-5 Criteria used to diagnose postpartum depression.
Universal screening for all pregnant and postpartum patients is highly recommended, and can be life-saving.
Bauman BL, Ko JY, Cox S, et al. Vital Signs: Postpartum Depressive Symptoms and Provider Discussions About Perinatal Depression — United States, 2018. MMWR Morb Mortal Wkly Rep 2020;69:575–581. DOI: http://dx.doi.org/10.15585/mmwr.mm6919a2
Category: Critical Care
Posted: 4/30/2024 by Quincy Tran, MD, PhD
(Updated: 5/3/2024)
Click here to contact Quincy Tran, MD, PhD
Title: Safety and Efficacy of Reduced-Dose Versus Full-Dose Alteplase for Acute Pulmonary Embolism: A Multicenter Observational Comparative Effectiveness Study
Settings: Retrospective observational study from a combination of Abbott Northwestern Hospital and 15 others as part of the Mayo Health system.
Participants: Patients between 2012 – 2020 who were treated for PE. Patients were propensity-matched according to the probability of a patient receiving a reduced- dose of alteplase.
Outcome measurement:
Study Results:
Discussion:
Conclusion:
In this retrospective, Propensity-score matching study, the full-dose regimen but is associated with a lower risk of bleeding.
Melamed R, Tierney DM, Xia R, Brown CS, Mara KC, Lillyblad M, Sidebottom A, Wiley BM, Khapov I, Gajic O. Safety and Efficacy of Reduced-Dose Versus Full-Dose Alteplase for Acute Pulmonary Embolism: A Multicenter Observational Comparative Effectiveness Study. Crit Care Med. 2024 May 1;52(5):729-742. doi: 10.1097/CCM.0000000000006162. Epub 2024 Jan 3. PMID: 38165776.
Category: Ultrasound
Keywords: Pleural Effusion; POCUS (PubMed Search)
Posted: 4/22/2024 by Alexis Salerno, MD
(Emailed: 4/29/2024)
(Updated: 4/29/2024)
Click here to contact Alexis Salerno, MD
How do you look for signs of a pleural effusion with ultrasound?
Place your ultrasound probe in the mid axillary line with the probe marker placed towards the patient's head.
Find the movement of the diaphragm and scan just above the diaphragm.
In normal lung, air scatters the ultrasound signal, and you are not able to see structures above the diaphragm.
With a pleural effusion, you can see:
Category: Cardiology
Posted: 4/28/2024 by Robert Flint, MD
Click here to contact Robert Flint, MD
In a cohort of 93,512 ED patients discharged with a diagnosis of hypertension there were 4400 who received a prescription for antihypertensives. The group receiving a prescription had fewer 30 day revisits and adverse events such as MI, CHF, etc.
Previous study’s have found it is safe to prescribe antihypertensives from the ED.
This study is limited by the fact it is not a randomized control trial and there are many variables as to why the select patients received prescriptions
The authors conclude: “Prescription antihypertensive therapy for discharged ED patients is associated with a 30-day decrease in severe adverse events and ED revisit rate.”
Brett R. Todd MD, Yuying Xing PhD, Lili Zhao PhD, An Nguyen MD, Robert Swor DO, Lauren Eberhardt, Amit Bahl MD
Journal of the American College of Emergency Physicians OpenVolume 5, Issue 2 e13138
Category: Orthopedics
Posted: 4/27/2024 by Brian Corwell, MD
(Updated: 5/3/2024)
Click here to contact Brian Corwell, MD
New progress in head injury prevention in football
A Guardian Cap is a soft padded soft shell worn over football helmets.
Think of it like a shock absorber
It is intended to mitigate energy transfer to the head and neck during player impacts.
It retails for about $70 on amazon!
https://www.pinkvilla.com/pics/855x855/236466742_untitled-design-2024-04-27t133219-626_202404.jpg
Most NFL players have worn these caps during preseason practices for the past 2 years.
The NFL found a 52% reduction in preseason concussions (at the same position) between players who wore the cap versus those who did not.
In laboratory testing the Guardian cap reduced head impact forces by up to 1/3rd in certain impacts.
Per NFL analytics, the Guardian cap absorbs 10% of the traumatic force.
Additionally, if two players suffer a helmet to helmet hit in which each wears the cap, the impact force is reduced by 20%!
The NFL has allowed players to wear the caps this year
They will have the team logos on them
2024 season: Players will wear the caps or one of 6 approved helmets (position specific) that provide equal or better protection.
If your child plays football, consider investing in this product as a potential means to reduce head impact forces and concussion.
More data is needed during regular season games with full speed collisions.
Category: Trauma
Posted: 4/24/2024 by Robert Flint, MD
(Updated: 5/3/2024)
Click here to contact Robert Flint, MD
A small study retrospectively looking at recorded calls to a level 1 trauma center transfer line specifically looking at patients who died or were discharged to hospice without surgical intervention found only 10% had goals of care discussed prior to transfer. Most were brain hemorrhage patients.
As a transferring facility, clearly outlining goals of care and addressing futility of care can have a major impact on trauma transfers and the cost and family burden associated with transfers.
Trenga-Schein, Nellie BA; Zonies, David MD, MPH, MBA, FACS, FCCM, FACHE; Cook, Mackenzie MD, FACS
Journal of Trauma and Acute Care Surgery 96(4):p 583-588, April 2024. | DOI: 10.1097/TA.0000000000004215
Category: Critical Care
Posted: 4/23/2024 by Caleb Chan, MD
Click here to contact Caleb Chan, MD
Background:
-Muscle rigidity has been described as a side-effect of fentanyl, specifically activation of expiratory muscles
-Excessive expiratory muscle use acts as “anti-PEEP,” causing lung derecruitment and hypoxemia
-End-expiratory lung volume (EELV) has been used as a surrogate for lung recruitment
Study:
-Small, two center, observational study (46 patients with ARDS)
-50% of patients had a significant increase in EELV after administration of neuromuscular blockade (NMB)
-Statistically significant correlation between a higher dosage of fentanyl and a greater increase in EELV after NMB
Takeaways:
-NMB can improve lung recruitment for a subset of patients with ARDS, particularly in patients with significant expiratory muscle use (this can be seen on your physical exam of your intubated ED boarding patient)
-Although this was not the main point of this study, consider fentanyl-associated “anti-PEEP,” particularly in patients receiving fentanyl whose hypoxemia and/or ventilator mechanics are disproportionate to their imaging
-This can be assessed with NMB (but ensure the patient will have adequate minute ventilation first)
-Naloxone has also been shown to reverse fentanyl-associated rigidity, but obviously would induce patient discomfort/withdrawal
*Of note, because this was an observational trial, it is possible that the patients with increased work of breathing were simply given more fentanyl. Regardless, these findings are consistent with previously documented physiologic side effects of fentanyl.
Plens GM, Droghi MT, Alcala GC, et al. Expiratory muscle activity counteracts positive end-expiratory pressure and is associated with fentanyl dose in patients with acute respiratory distress syndrome. Am J Respir Crit Care Med. 2024;209(5):563-572.
Category: Trauma
Posted: 4/21/2024 by Robert Flint, MD
Click here to contact Robert Flint, MD
PECARN has a decision tool to identify blunt trauma patients under age 18 who are low probability for important intra-abdominal injuries. The questions to ask are:
Answering no to all yields <0.1% chance of intra-abdominal trauma requiring intervention. (See MedCalc link for other calculations)
A prospective validation study in the Lancet yielded 100% sensitivity and negative predictive value in 7542 patients under age 18
This tool can likely be used to guide imaging choices in pediatric blunt abdominal trauma patients
Category: Pediatrics
Keywords: UTI, antibiotic, duration (PubMed Search)
Posted: 4/19/2024 by Jenny Guyther, MD
(Updated: 5/3/2024)
Click here to contact Jenny Guyther, MD
This was a multicenter, randomized double blind, placebo controlled, non inferiority trial looking at children aged 2 months to 10 years with a diagnosis of urinary tract infection to see if the antibiotic course could be shortened from 10 days to 5 days in those patients who have clinically improved by day 5.
Children were prescribed amoxicillin/clavulanic acid, cefixime, cefdinir, cephalexin or trimethoprim-sulfamethoxazole and on day 6, after an in person visit were switched to placebo or continued the same antibiotic course.
A urine sample was collected on days 11-14 and treatment failure was defined as symptomatic urinary tract infection at or before this visit, asymptomatic bacteriuria, positive urine culture or gastrointestinal colonization with resistant organisms.
693 children were randomized in this trial. Children who received 5 days of antibiotics were more likely to have asymptomatic bacteriuria or a positive urine culture on days 11-14 (0.6 vs 4.2%). 28 children would need to be treated with a 10 day course to prevent one treatment failure with the 5 day course.
Bottom line: 10 days is still the ideal duration of treatment for a urinary tract infection, but the rate of failure of a 5 day course was low and the clinical significance of asymptomatic bacteriuria or a positive urine culture in an otherwise asymptomatic child is unknown.
Zaoutis et al. Short-Course Therapy for Urinary Tract Infections in Children The SCOUT Randomized Clinical Trial. JAMA pediatrics. published online June 26, 2023.
Category: Administration
Keywords: staffing, employment, Teamhealth, Medstar, Edelman (PubMed Search)
Posted: 3/16/2024 by Steve Schenkel, MPP, MD
(Emailed: 4/17/2024)
(Updated: 4/17/2024)
Click here to contact Steve Schenkel, MPP, MD
Emergency Medicine staffing groups can be organized in any number of ways. Here’s Leon Adelman’s take:
Read more at https://emworkforce.substack.com/p/state-of-the-us-emergency-medicine-677. Read closely and you’ll find a reference to Maryland.
Category: Critical Care
Posted: 4/17/2024 by William Teeter, MD
(Updated: 4/24/2024)
Click here to contact William Teeter, MD
Moderate to High-Risk Pulmonary Embolism
In stable patients, call your local PE Response Team (PERT) for advice. The UMMC PERT team is available for any patient in the region and can be contacted through Maryland Access Center.
UMMC PERT stratifies by BOVA (with lactate criteria), CTA imaging, and patient physiology/history. For the consult, we will use the patients most recent vitals, their ROOM AIR sat if available, presence of RV dysfunction on echo/CTA, recent lactate, troponin, BNP, bedside/formal echo, and HPI.
Broad management recommendations for moderate or high-risk patients
PERT Acceptance for Transfer to UMMC/CCRU
See below for more information.
****************************************************************************************************************************************
Definitions of RV dysfunction
Absolute Contraindications to Fibrinolytic Therapy in Pulmonary Embolism
UMMC Relative Exclusion Criteria for VA ECMO for PE
HI-PEITHO (NCT04790370) “is a prospective, multicenter RCT comparing Ultrasound-facilitated catheter-directed therapy (USCDT) and best medical therapy (BMT; systemic anticoagulation) with BMT alone in patients with acute intermediate–high-risk PE.”
Inclusion Criteria
Category: EMS
Keywords: pediatric trauma, vital signs, blood pressure (PubMed Search)
Posted: 4/17/2024 by Jenny Guyther, MD
(Updated: 5/3/2024)
Click here to contact Jenny Guyther, MD
The short answer is yes, pediatric trauma patients without blood pressures recorded from EMS had a higher mortality (4.3%) compared to pediatric patients that did have a recorded blood pressure (1.1%). This is based off of a prehospital study conducted in Japan.
Prehospital vital signs are left out more often in pediatric patients compared to adults. Of those vital signs that are recorded, blood pressure is the most common one left off.
There can be several barriers to obtaining a blood pressure on the pediatric patient in the prehospital setting: lack of properly sized equipment, an uncooperative child, and lack of education. However, the inability to obtain a blood pressure can also be due to the patient being more severely injured and having other skills performed or was unable to be obtained due to poor perfusion. In this study, those who did not have a recorded blood pressure also had a lower GCS score and a higher injury severity score.
Shinohara et al. Association between blood pressure recording in prehospital setting and patient outcome in pediatric trauma patients: A prospective matching study. Journal of Trauma and Acute Care Surgery. July 2023. Epub ahead of print.
Category: Ultrasound
Keywords: POCUS; Lumbar Puncture; Neurology (PubMed Search)
Posted: 4/15/2024 by Alexis Salerno, MD
(Updated: 5/3/2024)
Click here to contact Alexis Salerno, MD
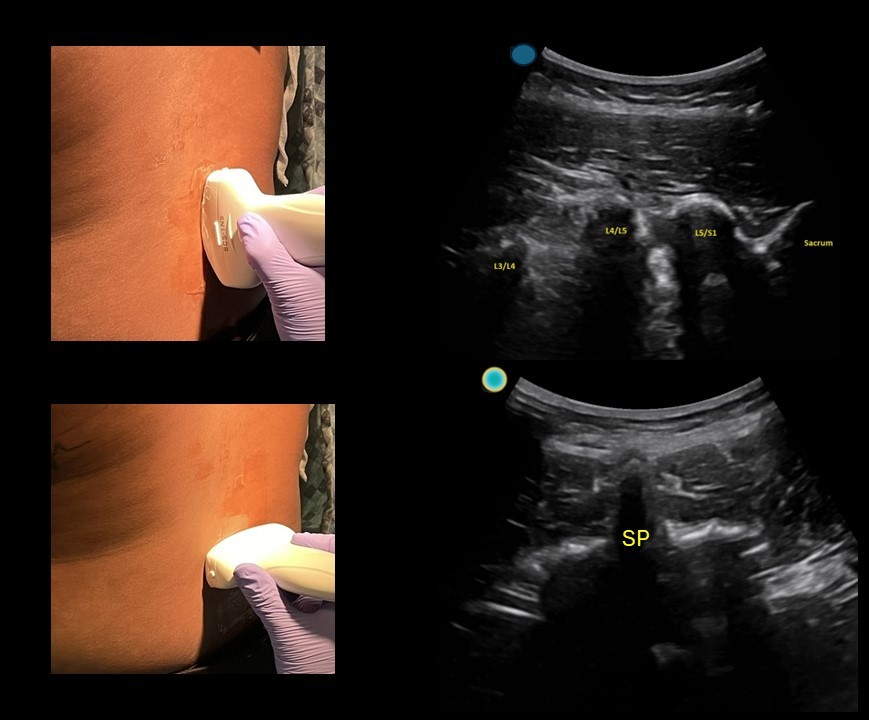
Simple tool to help improve your next lumbar puncture: Use ultrasound for site marking.
This can be done in a patient sitting up or laying on their side.
-First start with the probe marker midline towards the patient's head and use the ultrasound to identify the L4/L5 and L3/L4 space.
-Use a surgical pen away from the gel to mark midline on both sides of the probe, using the midline marker on the ultrasound probe. You can use m mode to help you identify the middle of the image when using a curvilinear probe.
-Then rotate the probe towards the patient's left and use the ultrasound to identify the midline point (spinous process)
-Use a surgical pen away from the gel to mark midline on both sides of the probe, using the midline marker on the ultrasound probe.
-Clean off the gel, connect the skin markings and use a 3 cc syringe to mark the center of the crosshair.
-Sterilize and start your LP!
Category: Trauma
Posted: 4/14/2024 by Robert Flint, MD
(Updated: 5/3/2024)
Click here to contact Robert Flint, MD
This study looked at survival pre and post implementation of an airway guideline for prehospital traumatic brain injury (TBI) patients who received positive pressure airway interventions. The guideline “focused on the avoidance and aggressive treatment of hypotension and 3 airway-related goals: (1) prevention or treatment of hypoxia through early, high-flow oxygen administration; (2) airway interventions to optimize oxygenation or ventilation when high-flow oxygen was insufficient; and (3) prevention of hyperventilation or hypocapnia by using ventilation adjuncts (ie, rate timers, flow-controlled ventilation bags, end-tidal carbon dioxide monitoring).”
Post implementation, survival to admission increased in all severity levels of TBI and in the most severely injured, survival to discharge improved.
Useful for those involved in prehospital education and as a reminder for in hospital airway management in TBI patients.
Gaither JB, Spaite DW, Bobrow BJ, et al. EMS Treatment Guidelines in Major Traumatic Brain Injury With Positive Pressure Ventilation. JAMA Surg. 2024;159(4):363–372. doi:10.1001/jamasurg.2023.7155
Category: Orthopedics
Posted: 4/14/2024 by Brian Corwell, MD
Click here to contact Brian Corwell, MD
Metacarpal fractures are frequently seen in the ED.
These are frequently non operative injuries.
For 4th and 5th metacarpal fractures, consider an ulnar gutter spilt.
For 2nd and 3rd metacarpal fractures, consider a radial gutter splint.
Splinting position (Intrinsic plus):
Wrist in approximately 20 degrees of extension (position of function)
MCP joint in 70 to 90 degrees of flexion
Slight flexion at the DIP and PIP and DIP joints.
-Important to prevent shortening of the collateral ligaments
Category: Pediatrics
Keywords: Pediatrics, preparedness (PubMed Search)
Posted: 4/5/2024 by Kathleen Stephanos, MD
(Emailed: 4/12/2024)
(Updated: 4/12/2024)
Click here to contact Kathleen Stephanos, MD
In early 2023 Newgard et al published an article in JAMA which looked at pediatric readiness in ED's across the county. This study showed that there was a significant increase in pediatric mortality in patients who presented to EDs with lower readiness scores (<87 out of 100) when compared to those with higher readiness scores. And this translated to not just the time in the ED, but up to a year after they are seen in an ill-prepared ED. This number equated to an estimated total of 1,500 preventable deaths in children in the US each year.
Notably this does NOT look at what designation your hospital has for pediatrics (so being a level 1 pediatric trauma center does not automatically give you any points). This is based on having the physical materials needed for each age group, plans in place for specific patient age groups and evaluations (lower radiation doses for children in CT, using an US before CT for appendicitis evaluation, etc), and a person/people in place to review cases and ensure everyone is up to date on pediatric related training.
Want to check YOUR score? Go to https://www.pedsready.org/
Newgard CD, Lin A, Malveau S, et al. Emergency Department Pediatric Readiness and Short-term and Long-term Mortality Among Children Receiving Emergency Care. JAMA Netw Open. 2023;6(1):e2250941. doi:10.1001/jamanetworkopen.2022.50941
Category: Pharmacology & Therapeutics
Keywords: naloxone, opioid (PubMed Search)
Posted: 4/11/2024 by Ashley Martinelli
(Updated: 5/3/2024)
Click here to contact Ashley Martinelli
Naloxone is given frequently in the emergency department to improve the respiratory rate in patients with suspected or known opioid ingestion. In order to minimize the risk of severe opioid withdrawal (nausea, vomiting, diarrhea, anxiety, piloerection, sweating, agitation, etc.), consider diluting naloxone and administering small aliquots of 0.04-0.08mg at a time. This requires IV access and a patient with a present, but low respiratory rate.
Dilution instructions:
Supplies:
Instructions:
Administer 1 -2 mL (0.04 – 0.08 mg) naloxone every 2 minutes and assess response.
Don't forget to prescribe/give naloxone upon discharge from the emergency department.
Category: Critical Care
Keywords: cardiac arrest, OHCA, airway, mechanical ventilation, resuscitation, bag-valve mask, manual ventilation (PubMed Search)
Posted: 4/10/2024 by Kami Windsor, MD
Click here to contact Kami Windsor, MD
In cardiac arrest, avoidance of excessive ventilation is key to achieving HQ-CPR and minimizing decreases in venous return to the heart. The controversy regarding BVM vs definitive airway and OHCA outcomes continues, but data indicates that mechanical ventilation during CPR carries no more variability in airway peak pressures and tidal volume delivery than BVM ventilation [1], with the AHA suggestion to keep in-hospital cardiac arrest patients with COVID-19 on the ventilator during the pandemic [2].
So, can we automate this part of CPR?
Two recent studies looked at mechanical ventilation (MV) compared to bagged ventilation (BV) in intubated patients with out-of-hospital-cardiac arrest (OHCA).
Shin et al.'s pilot RCT evaluated 60 intubated patients, randomizing half to MV and half to BV, finding no difference in the primary outcome of ROSC or sustained ROSC, or ABG values, despite significantly lower tidal volumes and minute ventilation in the MV group [3].
Malinverni et al. retrospectively compared MV and BV OHCA patients from the Belgian Cardiac Arrest Registry, finding that MV was associated with increased ROSC although not with improved neurologic outcomes. Of note, patients across the airway spectrum were included (mask, supraglottic, intubated), and the mechanical ventilation was a bilevel pressure mode called Cardiopulmonary Ventilation (CPV) specific to their ventilators, specifically for use during cardiac arrest [4].
Bottom Line: Larger randomized trials will be necessary to get a definitive answer as to how mechanical ventilation affects outcomes in OHCA, but in instances where the cause of arrest is not primarily pulmonary (severe asthma, pneumothorax) and the ED is short-staffed or prolonged resuscitations are likely (such as in accidental hypothermic arrests), it is probably reasonable to keep patients on the ventilator:
Category: Trauma
Keywords: Trauma, blood pressure, shock index, predictor, mortality (PubMed Search)
Posted: 4/8/2024 by Robert Flint, MD
Click here to contact Robert Flint, MD
Traditionally, a systolic blood pressure (SBP) of 90 has been used as a marker of severe illness in trauma patients. This study looked at a large database and found shock index (SI) and systolic blood pressure were the best predictors of early mortality in trauma patients.
They found:
prehospital SI 0.9 and SBP 110,
ED SI 0.9 and SBP 112,
and
in elderly
prehospital SI 0.8 SBP 116
ED SI 0.8 SBP 121
were the cutoffs to predict early mortality.
We should rethink our protocols and approach to trauma patients using a higher systolic blood pressure than 90. Also note elderly had a different number than younger trauma patients.
April MD, Fisher AD, Rizzo JA, Wright FL, Winkle JM, Schauer SG. Early Vital Sign Thresholds Associated with 24-Hour Mortality among Trauma Patients: A Trauma Quality Improvement Program (TQIP) Study. Prehosp Disaster Med. 2024 Apr 2:1-5. doi: 10.1017/S1049023X24000207. Epub ahead of print. PMID: 38563282.
