Category: Pediatrics
Keywords: neonatal fever, cellulitis, bacteremia (PubMed Search)
Posted: 6/16/2023 by Jennifer Guyther, MD
(Updated: 5/17/2024)
Click here to contact Jennifer Guyther, MD
Kaplin, Ron. Clinical Presentation and Approach to Evaluation and Management. Pediatric Emergency Care 2023; 39(3):188-189.
Category: Toxicology
Keywords: Lithium, Lab error, Toxicity (PubMed Search)
Posted: 6/15/2023 by Natasha Tobarran, DO
(Updated: 5/17/2024)
Click here to contact Natasha Tobarran, DO
Lithium toxicity can present acutely with gastrointestinal symptoms and chronically with neurologic symptoms such as tremor and ataxia. Diagnosis and treatment with normal saline hydration and/or dialysis depends on lithium levels in conjunction with signs and symptoms.
Lithium levels can be falsely elevated when blood samples are collected in green top tubes which contain lithium heparin, or if the blood collection volume is too small. Not recognizing that a lithium level may be falsely elevated can lead to misdiagnosis as well as unnecessary hospitalizations and treatments. The study by Wills et al found lithium levels as high as 4 mmol/L (therapeutic range 0.6-1.2 mmol/L) in lithium naïve volunteers collected in the wrong tube and with small blood volumes. If a patient has an elevated lithium level in the absence of lithium toxicity symptoms, consider a falsely elevated level and redraw using the appropriate tube and sample size.
In summary:
Wills BK, Mycyk MB, Mazor S, Zell-Kanter M, Brace L, Erickson T. Factitious lithium toxicity secondary to lithium heparin-containing blood tubes. J Med Toxicol. 2006 Jun;2(2):61-3. doi: 10.1007/BF03161172. PMID: 18072115; PMCID: PMC3550057.
Category: Administration
Keywords: STEMI, pericarditis, (PubMed Search)
Posted: 6/11/2023 by Leen Alblaihed, MHA, MBBS
(Emailed: 6/12/2023)
Click here to contact Leen Alblaihed, MHA, MBBS
a 37 year old patient comes in with chest pain, you obtain the following ECG. Is this a STEMI or Pericarditis?
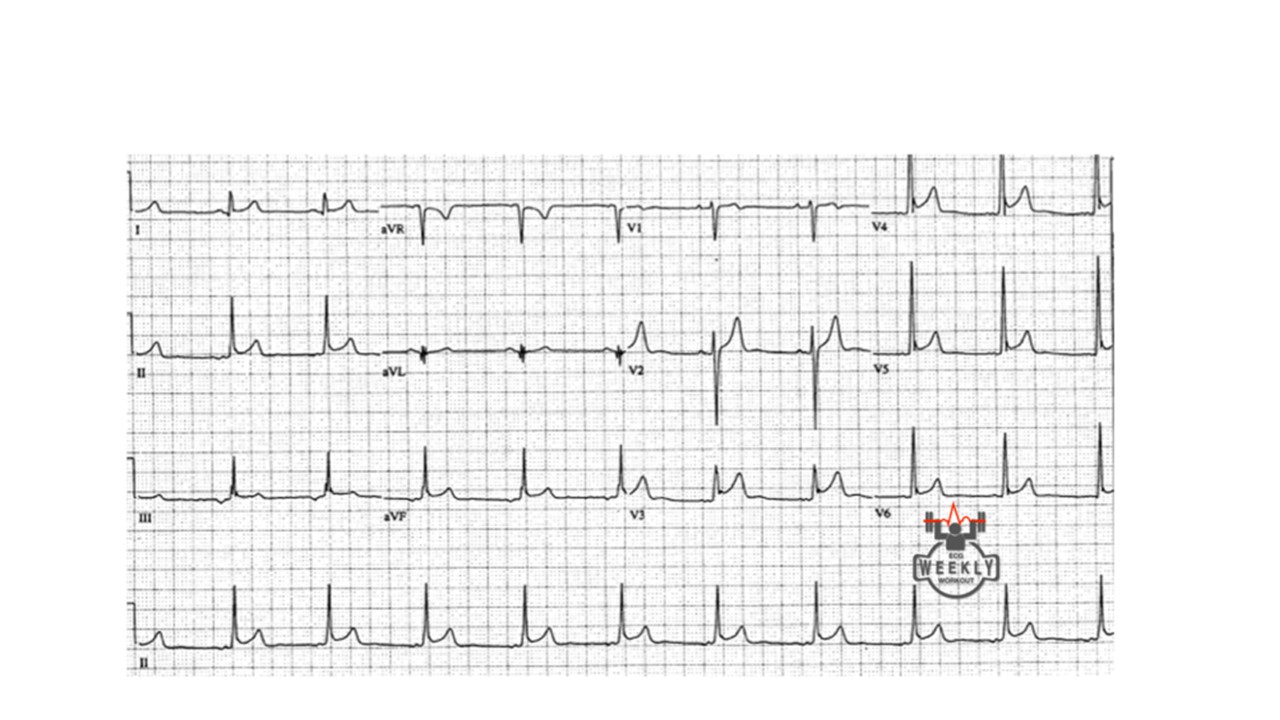
How can you tell? well, you follow the algorithm Dr. Mattu taught us....
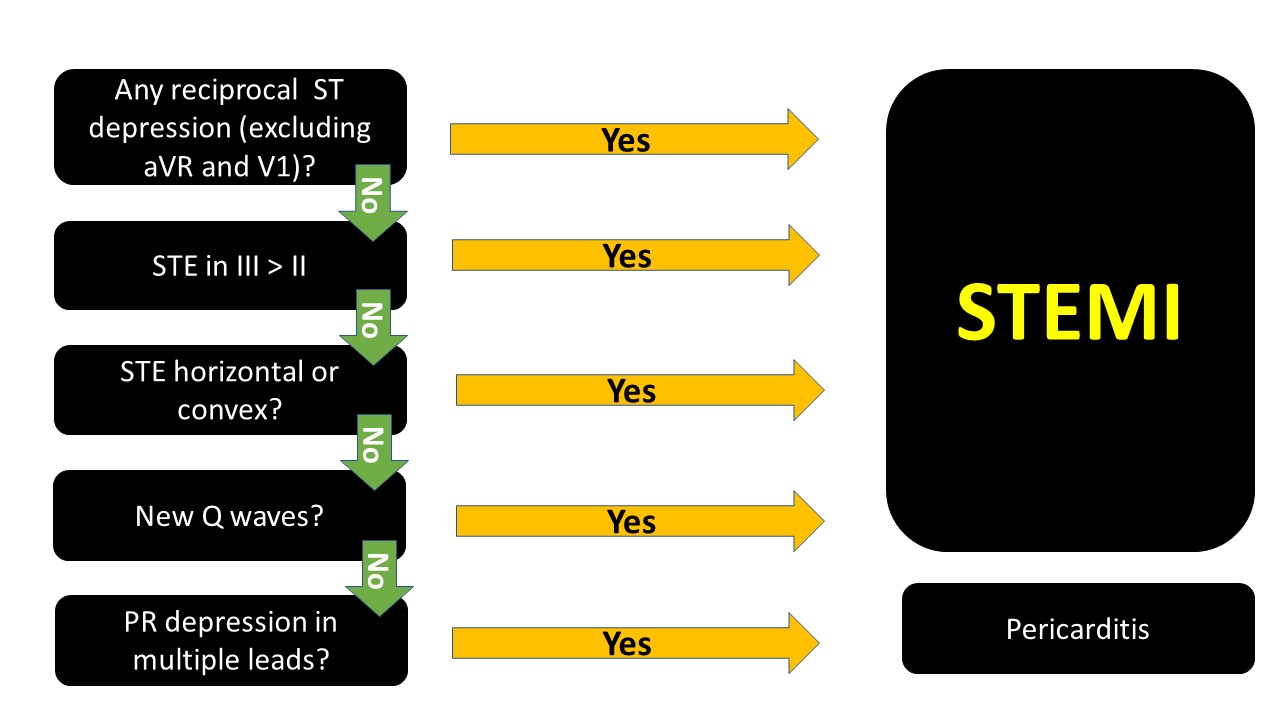
The ECG above, if you go through the algorithm you will see that it is most likely pericarditis.
note that PR depression can be transient and you might not see them.
When in doubt, it is not wrong to consult cardiology. Getting serial ECGs also is important, STEMIs will usually evolve.
Category: Trauma
Keywords: thoracotomy, survival, prognosis (PubMed Search)
Posted: 6/9/2023 by Robert Flint, MD
(Emailed: 6/11/2023)
Click here to contact Robert Flint, MD
Recognizing that the studies discussing emergency department thoracotomy (ERT) in traumatic injuries are performed at large institutions where surgical back-up is available, emergency physicians should be familiar with the indications of emergency department thoracotomy in the setting of trauma. An informed decision should be made based on resources available along with the limited literature available to make the best decision for the patient and staff present.
Adding to last week’s pearl of no cardiac activity and no pericardial fluid on FAST exam, what else prognosticates intact survival? A 2020 paper concluded “ERT had the highest survival rates in patients younger than 60 years who present with signs of life after penetrating trauma. None of the patients with blunt trauma who presented with no signs of life survived.” 1A review in Trauma last month recommended: “Based on our scoping review of existing literature, we can conclude three major findings in the context of RT: (1) Resuscitative Thoracotomies (RT) performed in the setting of blunt trauma have a worse prognosis compared to patients undergoing RT for penetrating injuries, (2) procedures that have the potential to delay patient transport to hospital, such as intubation, may significantly increase the risk of mortality and (3) the presence of signs of life or hemodynamic stability in the prehospital or in-hospital setting are positive survival predictors in the setting of RT” 2 The best outcome is in patients brought immediately to an ED (preferably a trauma center) with limited on scene time. Police transport had a major association with survival in these patients. Stab wounds have the highest rate of intact survival.
For those at non-trauma centers, have a conversation within your ED group as well as with general surgeons (if available) to decide ahead of time if this procedure will be utilized in the setting of traumatic cardiac arrest and in which patient population.
1. Vahe S Panossian , Charlie J Nederpelt , Majed W El Hechi , David C Chang , April E Mendoza , Noelle N Saillant , George C Velmahos Haytham M A Kaafarani Emergency Resuscitative Thoracotomy: A Nationwide Analysis of Outcomes and Predictors of Futility J Surg Res. 2020 Nov;255:486-494. doi: 10.1016/j.jss.2020.05.048. Epub 2020 Jul 1.
2. Radulovic N, Wu R, Nolan B. Predictors of survival in trauma patients requiring resuscitative thoracotomy: A scoping review. Trauma. 2023;0(0). doi:10.1177/14604086231156265
Category: Orthopedics
Keywords: shoulder, Adhesive capsulitis (PubMed Search)
Posted: 6/10/2023 by Brian Corwell, MD
Click here to contact Brian Corwell, MD
Adhesive capsulitis aka frozen shoulder
Definition: Gradual development of global limitation of both active and passive shoulder motion, characterized by severe pain and lack of radiographic findings
Idiopathic loss of BOTH active and passive motion (significant reduction of at least 50%)
Motion is stiff and painful especially at the extremes.
Occurs due to thickening and contracture of the shoulder capsule.
Affects up to 8-10% of people of working age.
Affects patients between the ages of 40 and 60.
Peak age mid 50s
Onset before 40 is rare (consider other diagnosis).
Affects women more than men.
Diabetes is the most common risk factor.
Patients with DM, suffer a more prolonged course and are more resistant to therapy
Also associated with thyroid disease and prolonged immobilization
Increased risk following trauma to shoulder region (rotator cuff tear, following shoulder surgery, fracture of proximal humerus)
Presents unilaterally (other shoulder may become involved in next 5 years)
Slight increased risk of non-dominant shoulder
Category: Airway Management
Keywords: hypotension, pharmacology, RSI (PubMed Search)
Posted: 6/9/2023 by Robert Flint, MD
(Updated: 5/17/2024)
Click here to contact Robert Flint, MD
Take away: Be prepared (with blood products and/or vasopressors) for hypotension in trauma patients post-intubation particularly the elderly and severely injured. Pre-intubation tachycardia predicts post-intubation hypotension. Resuscitation with saline in traumatically injured patients is inferior to blood products or permissive hypotension.
A UK study retrospectively looked at trauma patients undergoing helicopter based emergency medicine intubation using induction agents of fentanyl, ketamine, and rocuronium for hypotensive episodes. “This study demonstrates that more than one in five patients who undergo PHEA have a new episode of significant hypotension within the first ten minutes of induction. Increasing patient age, multi-system injuries, a higher baseline heart rate, and intravenous crystalloid administration by the ambulance service before HEMS arrival were all significantly associated with PIH, whereas the addition of fentanyl to the induction drug regime was not.”
Price, J., Moncur, L., Lachowycz, K. et al. Predictors of post-intubation hypotension in trauma patients following prehospital emergency anaesthesia: a multi-centre observational study. Scand J Trauma Resusc Emerg Med 31, 26 (2023). https://doi.org/10.1186/s13049-023-01091-z
Category: Pharmacology & Therapeutics
Keywords: nitroglycerin, administration set, drug sorption, PVC tubing, polyethylene, SCAPE (PubMed Search)
Posted: 6/8/2023 by Matthew Poremba
(Updated: 5/17/2024)
Click here to contact Matthew Poremba
Nitroglycerin easily migrates into polyvinyl chloride (PVC), a plastic commonly used in intravenous tubing due to its flexibility and low cost. A slow rate of flow and long tubing length increase the loss of nitroglycerin. While using less absorptive tubing (i.e. polyethylene or polypropylene) when administering nitroglycerin is recommended, most published clinical studies looking at nitroglycerin have used PVC tubing.
A 1989 study compared nitroglycerin delivery through PVC tubing and low sorbing tubing at various concentrations and flow rates.1 Samples were obtained from the nitroglycerin bottle and the distal end of the tubing at several time points.
A 2018 study enrolled 8 volunteers to receive nitroglycerin infusions through PVC tubing and low sorbing polyolefin tubing.2
Bottom Line: Most studies evaluating nitroglycerin use in various clinical scenarios have used PVC tubing. Doses based on use with PVC tubing may be too high when using less absorptive tubing. Employing more conservative dosing strategies when using low sorbing tubing can help mitigate the risk of adverse effects (i.e. hypotension, headache).
Category: Critical Care
Keywords: Upper GI Hemorrhage, Cirrhosis, Antibiotic Prophylaxis, SBP, ceftriaxone (PubMed Search)
Posted: 6/6/2023 by Zach Rogers, MD
(Updated: 5/17/2024)
Click here to contact Zach Rogers, MD
Prophylactic antibiotic use in cirrhotic patients with an upper GI bleed has been demonstrated to have a mortality benefit in multiple randomized clinical trials. Some trials as well demonstrated a decreased risk of rebleeding as well as a shorter hospital length of stay (1,2).
The exact means of protection is not entirely clear and its benefit is seen in both variceal and nonvariceal hemorrhages as well as in cirrhotic patient both with and without ascites.
There does appears to be a close interplay between cirrhosis bleeding risk and infection, with infection being a common precipitating factor for upper GI bleed.
The antibiotic of choice is ceftriaxone 1 gram IV daily for seven days. Although in case of allergy/intolerance, fluoroquinolones or aminoglycosides may be used as alternatives (3).
Bottom line:
All forms of upper GI hemorrhage in cirrhotic patients warrant prophylactic antibiotic use (regardless of the presence of ascites) as well as a diligent search and exclusion of possible infectious sources.
1. Chavez-Tapia NC, Barrientos-Gutierrez T, Tellez-Avila FI, Soares-Weiser K, Uribe M. Antibiotic prophylaxis for cirrhotic patients with upper gastrointestinal bleeding. Cochrane Database Syst Rev. 2010 Sep 8;2010(9):CD002907. doi: 10.1002/14651858.CD002907.pub2. PMID: 20824832; PMCID: PMC7138054.
2. Wong YJ, Tan CK, Yii YL, et al. Antibiotic prophylaxis in cirrhosis patients with upper gastrointestinal bleeding: An updated systematic review and meta?analysis. Portal Hypertension & Cirrhosis. 2022;1(3):167-177. doi:10.1002/poh2.35
3. Sanchez?Jimenez B, Chavez?Tapia NC, Jakobsen JC, Nikolova D, Gluud C. Antibiotic prophylaxis for people with cirrhosis and variceal bleeding. Cochrane Database Syst Rev. 2018 Dec 4;2018(12):CD013214. doi: 10.1002/14651858.CD013214. PMCID: PMC6517118.
Category: Orthopedics
Keywords: POCUS, Knee Pain, Tendon Rupture (PubMed Search)
Posted: 6/5/2023 by Alexis Salerno, MD
Click here to contact Alexis Salerno, MD
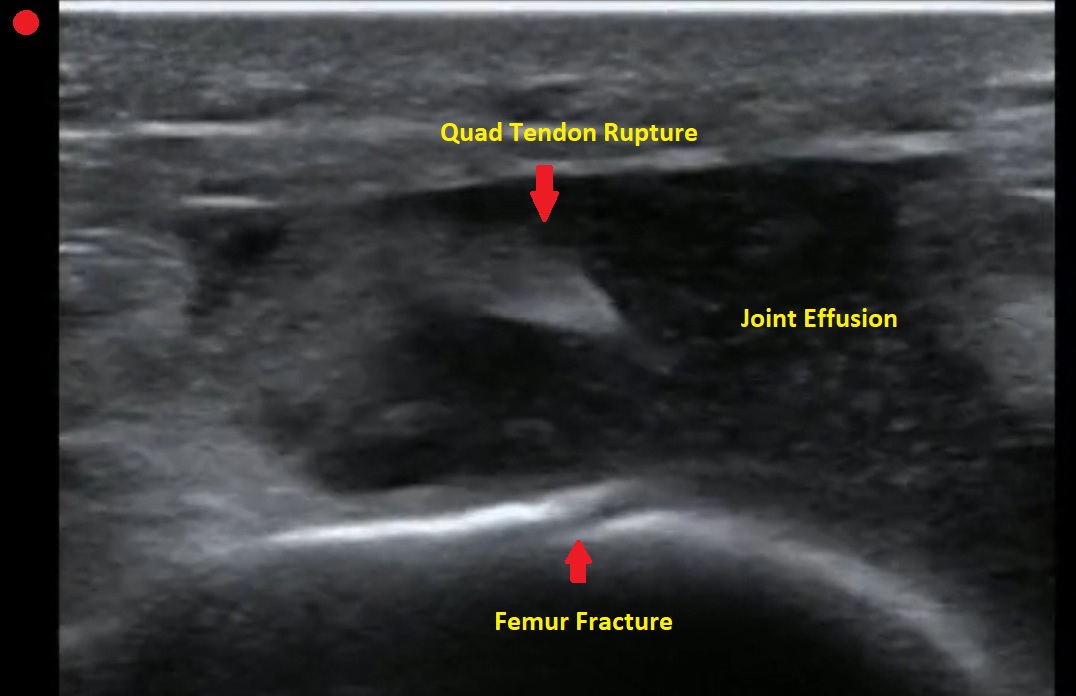
Pt presents to the emergency department with knee pain.
You decide to ultrasound the proximal knee. You place your ultrasound probe in the midline of the knee with your probe marker towards the patient's head.
What is the diagnosis?
-
--
---
--
-
The answer is a quadriceps tendon rupture with femur fracture.
Category: Trauma
Keywords: thoracotomy, REBOA, FAST, survival (PubMed Search)
Posted: 6/4/2023 by Robert Flint, MD
(Updated: 5/17/2024)
Click here to contact Robert Flint, MD
Bottom Line: Lack of pericardial fluid or cardiac motion on FAST exam leads to no intact survivors for ED RT for trauma.
Zone 1 REBOA may be as good or better than ED RT for those requiring aortic occlusion after trauma.
Intact neurologic survival after emergency department resuscitative thoracotomy (ED RT) for trauma is low. Best outcomes have been shown for stab wounds to the chest with loss of vital signs in the ED or just prior to ED arrival. Worst outcomes are for blunt trauma with loss of vital signs in the field.
Two studies help us further evaluate the use of emergency department resuscitative thoracotomy. Inaba et al. illustrate in patients undergoing a FAST exam prior to or concomitant with ED RT “The likelihood of survival if pericardial fluid and cardiac motion were both absent was zero.” Cralley et al. compared survival after ED RT to Resuscitative Endovascular Balloon Occlusion of the Artery (REBOA) zone 1 (above celiac axis) and found REBOA was as good or better when used in centers with experience with both procedures. They advocate for a randomized trial to compare the two procedures further.
Inaba, Kenji MD*; Chouliaras, Konstantinos MD*; Zakaluzny, Scott MD*; Swadron, Stuart MD†; Mailhot, Thomas MD†; Seif, Dina MD†; Teixeira, Pedro MD*; Sivrikoz, Emre MD*; Ives, Crystal MD*; Barmparas, Galinos MD*; Koronakis, Nikolaos MD*; Demetriades, Demetrios MD*. FAST Ultrasound Examination as a Predictor of Outcomes After Resuscitative Thoracotomy: A Prospective Evaluation. Annals of Surgery 262(3):p 512-518, September 2015. | DOI: 10.1097/SLA.0000000000001421
Alexis L. Cralley, MD1; Navin Vigneshwar, MD, MPH1; Ernest E. Moore, MD1,2; et al
Zone 1 Endovascular Balloon Occlusion of the Aorta vs Resuscitative Thoracotomy for Patient Resuscitation After Severe Hemorrhagic Shock JAMA Surg. 2023;158(2):140-150. doi:10.1001/jamasurg.2022.6393
Category: Quality Assurance/Quality Improvement
Keywords: Emergency Department Boarding, Emergency Department Crowding (PubMed Search)
Posted: 6/3/2023 by Brent King
Click here to contact Brent King
The authors of this study retrospectively compared the 10-day mortality rates of patients who were triaged to levels 3-5 on the Scandinavian Rapid Emergency Triage and Treatment System (RETTS) during times of ED crowding (as measured by length of stay and percentage bed occupancy) with those who came to the ED at other times.
Patients were divided into four quartiles, corresponding with 2-hour length of stay blocks with quartile one having a length of stay of 2 or fewer hours and quartile four having a length of greater than 8 hours
Results: 705,076 patients were seen in one of two EDs from 2009 to 2016. The 10-day mortality rate was 0.09% (n = 623). The authors found an increased 10-day mortality for patients in quartile four as compared to those in quartile one “(adjusted odds ratio 5.86; 95% confidence interval [CI] 2.15 to 15.94)” This was also true for times when the ED occupancy ratio was greater than one (more than one patient in the ED per available bed). “Adjusted odds ratios for ED occupancy ratio quartiles 2, 3, and 4 versus quartile 1 were 1.48 (95% CI 1.14 to 1.92), 1.63 (95% CI 1.24 to 2.14), and 1.53 (95% CI 1.15 to 2.03), respectively”
Older patients and those with co-morbidities were at greatest risk but lower-acuity patients in all age and morbidity classes had an increased risk of death within 10 days if they came to the ED when it was crowded.
The RETTS Triage System as Described by the Authors:
A “ 5-level triage scale descending from red (1) to blue (5), in which red represents the most urgent level. RETTS is based on one main principle: whether the patient is assessed as unstable or stable during triage. Unstable patients are experiencing potentially life-threatening conditions and are allocated to 1 of the 2 highest triage levels (1 to 2), whereas stable patients are allocated to 1 of the 3 lowest triage levels (3 to 5). Stable patients need medical attention but are considered able to wait because they are not at any obvious medical risk. RETTS uses a combination of vital signs and 59 chief complaint algorithms to allocate the triage level. The vital signs have cutoff levels for each triage level, and the chief complaint algorithms are known as emergency symptoms and signs for emergency care. Each emergency symptom and sign includes one or more chief complaints and is classified according to the International Statistical Classification of Diseases and Related Health Problems, 10th Revision, 2007 (ICD-10), and a logistic process is attached to each algorithm”
The authors state that the RETTS system cannot be directly compared to the ESI system used in much of the US but they believe that RETTS levels 3-5 roughly correspond to levels 4 and 5 in the Canadian Triage and Acuity Scale.
Berg LM, Ehrenberg A, Florin J, et al. Associations Between Crowding and Ten-Day Mortality Among Patients Allocated Lower Triage Acuity Levels Without Need of Acute Hospital Care on Departure From the Emergency Department Ann Emerg Med. 2019;74:345-356.
Category: Pediatrics
Keywords: congenital heart disease (PubMed Search)
Posted: 6/2/2023 by Rachel Wiltjer, DO
Click here to contact Rachel Wiltjer, DO
Some things are easy, even reflexive, and one of those things is putting oxygen on cyanotic patients. Usually, this is a great thing. Blue = bad. Occasionally, though, blue = baseline and even in those patients who are too blue, you want to keep them closer to purple than pink.
This issue is commonly encountered in certain types of congenital heart disease and as well as through various phases of their repair. These include ductal dependent lesions, those with significant shunts, and single ventricle physiology. Oxygen functions as a pulmonary vasodilator and can increase or change the direction of shunting, directly impacting physiology by causing pulmonary overcirculation, increased strain on the right ventricle, and decreases in systemic circulation.
Helpful Hints:
1) Find out and shoot for the patient’s goal oxygen saturation range (many lesions will be 75%-85%). This may be available from parents, in the EMR, or by calling the child’s cardiac center if they are an established patient.
2) In an undiagnosed neonate with hypoxia and signs of heart failure (crackles, enlarged liver, edema to the sacrum and/or occiput) or if unresponsive to initial trial of oxygen, decrease FiO2 and titrate support (nasal cannula with blender to set FiO2, HFNC, NIPPV, or intubation if necessary) to address respiratory distress as well as evaluation and treatment for ductal dependent lesions.
3) You may still need to use additional FiO2 to obtain reasonable oxygen saturations, but titrate thoughtfully.
Khalil M, Jux C, Rueblinger L, Behrje J, Esmaeili A, Schranz D. Acute therapy of newborns with critical congenital heart disease. Transl Pediatr. 2019 Apr;8(2):114-126.
McMann, K. T, Schelonka R.L. Editorial: Oxygen for cyanotic neonates: Friend or foe? Pediatric Health. 2010 Feb; 4(1): 1-3.
Category: Toxicology
Keywords: amlodipine, non-dihydropyridines, high-dose insulin (PubMed Search)
Posted: 6/1/2023 by Hong Kim, MD
(Updated: 5/17/2024)
Click here to contact Hong Kim, MD
Calcium channel blocker (CCB) overdose can lead to severe shock/hypotension. A small study was conducted to compare the hemodynamic effects of high-dose insulin (HDI) for two classes of CCB (dihydropyridines vs. non-dihydropyridines) that work differently to manage hypertension.
Study design:
Study sample:
Result
Median number of maximum concomitant vasopressors (p=0.04)
Median difference in max concomitant vasopressors: 1 (95% CI: 0 – 2)
Median max epinephrine dosing
Use of rescue methylene blue (p=0.009)
Conclusion:
Cole JB, Lee SC, Prekker ME, Kunzler NM, Considine KA, Driver BE, Puskarich MA, Olives TD. Vasodilation in patients with calcium channel blocker poisoning treated with high-dose insulin: a comparison of amlodipine versus non-dihydropyridines. Clin Toxicol (Phila). 2022 Nov;60(11):1205-1213. doi: 10.1080/15563650.2022.2131565. Epub 2022 Oct 25. PMID: 36282196.
Category: Trauma
Keywords: pain control, fentanyl, oral medication, trauma (PubMed Search)
Posted: 5/31/2023 by Robert Flint, MD
(Updated: 5/17/2024)
Click here to contact Robert Flint, MD
A study looking at 177 trauma patients (predominately skiing injuries) treated with oral trans mucosal fentanyl (600 and 800 mcg dosing) found a statistically and clinically significant reduction in pain. This therapy could be an adjunct to patients who require pain relief but IV access is delayed for various reasons.
Pietsch, U., Fischer, H., Rüst, C.A. et al. Oral transmucosal fentanyl citrate analgesia in prehospital trauma care: an observational cohort study. Scand J Trauma Resusc Emerg Med 31, 2 (2023). https://doi.org/10.1186/s13049-023-01066-0
Category: Critical Care
Keywords: thrombocytopenia, bleeding, hemorrhage, platelets, transfusions, central lines, CVCs (PubMed Search)
Posted: 5/30/2023 by Kami Windsor, MD
Click here to contact Kami Windsor, MD
Background: In general practice, platelets are typically transfused for invasive procedures when the platelet count falls below 50 x 109/L. Regarding the placement of central venous catheters (CVCs), there is minimal data to support or refute decisions to transfuse platelets in these patients, although the 2015 Clinical Practice Guideline from the AABB (formerly, the American Association of Blood Banks) recommends deferring platelet transfusion until a platelet count of 20 x 109/L for CVC placement [weak recommendation, low quality evidence].1
In a study published this month in NEJM,2 van Baarle et al. performed a multicenter randomized controlled noninferiority trial comparing platelet transfusion to no transfusion in patients with platelets 10 to 50 x 109/L prior to US-guided CVC insertion. The primary outcome was the occurrence of catheter-related bleeding Grades 2-4 (Grade 1 = oozing; managed with <20 min of manual compression, not requiring RBC transfusion, & Grades 2-4 is everything else up to death) within 24 hours post-procedure.
Bottom Line: The jury is still out on best platelet transfusion practices prior to CVC placement, but I would strongly consider prophylactic platelet transfusion in patients with platelets < 30 x 109/L, those with underlying hematologic malignancy, and patients receiving larger CVCs such as dialysis lines. How much to transfuse in those with more severe thrombocytopenia is uncertain.
Separately, I would also strongly recommend use of US-guidance for any CVC placement in this population as well, based on practical common sense and some supportive literature as well.5
Additional Background: Data in pediatric oncology patients indicates that CVC placement with platelets <50 x 109/L is associated w/ increased occurence of minor but not major post-procedure bleeding,3 while adult data indicates that CVC placement can be performed until a threshold of 20 x 109/L before transfusions are needed to prevent severe bleeding.4
Additional Study Data:
Category: Administration
Keywords: POCUS, Lung Ultrasound, Pneumothorax (PubMed Search)
Posted: 5/29/2023 by Alexis Salerno, MD
Click here to contact Alexis Salerno, MD
We hope that you enjoy your Memorial Day!
Don't forget your Sandy Beach Sign vs Barcode Sign of Lung Ultrasound:
Normal lung will have good pleural sliding. When you image the lung with M-Mode it looks like a Sandy Beach.
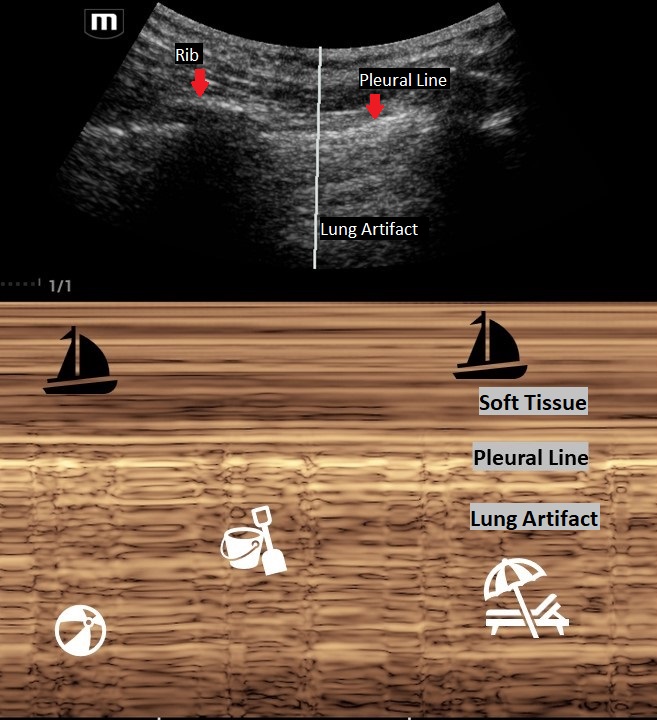
A lung with a pneumothorax will have poor lung sliding. When you image the lung with M-Mode it looks like a classic barcode or "stratosphere sign."
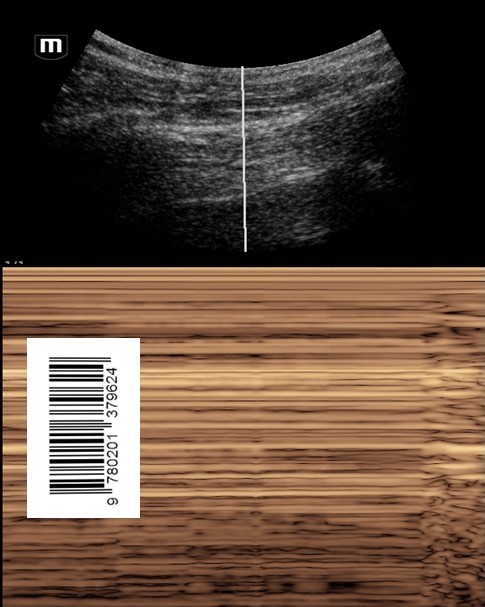
Make sure that you are on "Lung Mode" or decrease the gain to better image the movement of the pleural line. The negative predictive value for lung sliding on ultrasound is 99%. This means that if you see lung sliding you do not have a pneumothorax in that area. However, lung sliding is affected by certain conditions such as blebs, pulmonary fibrosis, pleural adhesions and right mainstem intubation. So, like any other radiology study, clinically correlate!
Thinking about placing a chest tube or have a patient with multiple rib fractures? Take a look at how to perform a Serratus Anteror Plane Block here: https://www.thepocusatlas.com/thoracoabdominal-blocks#Serratus
Husain LF, Hagopian L, Wayman D, Baker WE, Carmody KA. Sonographic diagnosis of pneumothorax. J Emerg Trauma Shock. 2012 Jan;5(1):76-81. doi: 10.4103/0974-2700.93116. PMID: 22416161; PMCID: PMC3299161.
Category: Trauma
Keywords: firearm, death, suicide, intentional, (PubMed Search)
Posted: 5/25/2023 by Robert Flint, MD
(Emailed: 5/28/2023)
(Updated: 5/17/2024)
Click here to contact Robert Flint, MD
This study looked at 20 years of death by firearm and stratified the location of death from urban to rural. The authors concluded:
“Descriptively, in all county types and both decades of the study, per capita gun suicides were more common than per capita gun homicides, and the most rural counties had higher rates of firearm death compared with the most urban counties. Firearm death rates were meaningfully higher in 2011-2020 compared with 2001-2010, primarily because of an increase in gun suicides.”
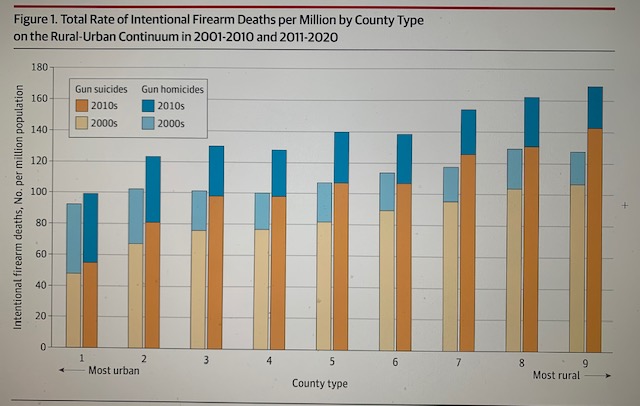
Paul M. Reeping, PhD1; Allison Mak, MD2,3; Charles C. Branas, PhD1; et al
Firearm Death Rates in Rural vs Urban US Counties
JAMA Surg. Published online April 26, 2023. doi:10.1001/jamasurg.2023.0265
Category: Orthopedics
Keywords: overuse injury, wrist (PubMed Search)
Posted: 5/25/2023 by Brian Corwell, MD
(Emailed: 5/27/2023)
Click here to contact Brian Corwell, MD
Intersection syndrome
Intersection syndrome is an overuse injury of the forearm.
Pain is located approximately 2 finger breaths (4cm) proximal to the wrist joint.
https://www.sportsmedreview.com/wp-content/uploads/2020/11/intersectionsyndrome.png
Mechanism: friction is caused by repetitive wrist extension activities
Commonly: Rowing, skiing, tennis, canoeing and weightlifting
Friction may cause crepitus with finger/wrist extension.
Tenderness, mild swelling may be present
Category: Visual Diagnosis
Keywords: C Spine, osteomyelitis, (PubMed Search)
Posted: 5/25/2023 by Robert Flint, MD
(Updated: 5/17/2024)
Click here to contact Robert Flint, MD


Neck pain and trouble swalowing. No trauma.
Osteomyelitis of the cervical spine is the least common location to find spinal infection. “Osteomyelitis of the cervical spine is a rare disease, representing only 3% – 6% of all cases of vertebral osteomyelitis. In contrast with other locations of spinal infections, osteomyelitis of the cervical spine can be a much more dramatic and rapidly deteriorating process, leading to early neurologic deficit”.
Note the bony destruction as well as the abscess labeled on the lateral view.
Category: Administration
Keywords: patient experience, clinician wellbeing (PubMed Search)
Posted: 5/24/2023 by Mercedes Torres, MD
Click here to contact Mercedes Torres, MD
Clinician Well-Being and the Patient Experience
Did you know that most patient experience responses are overwhelmingly positive? Rather than focusing all our attention on the bad, let’s focus on the good to promote clinician well-being. See below for a few key points from a recent study on this:
Consider emphasizing positive patient experiences when providing feedback to emergency physicians. It will promote clinician well-being and help improve performance in your practice.
Dudley J and Lee TH. Patient Experience and Clinician Well-Being Aren’t Mutually Exclusive. Harvard Business Review. Published online at hbr.org, July 18, 2022.
